The blood pressure in your body depends upon the following conditions:
- The force of contraction of the heart -- related to how much the heart muscle gets stretched by the incoming blood.
- The degree to which the arteries and arterioles constrict -- increases the resistance to blood flow, thus requiring a higher blood pressure.
- The circulating blood volume -- the higher the circulating blood volume, the more the heart muscle gets stretched by the incoming blood.
The kidney influences blood pressure by:
- Causing the arteries and veins to constrict
- Increasing the circulating blood volume
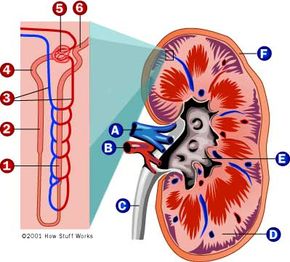
Specialized cells are located in a portion of the distal tubule located near and in the wall of the afferent arteriole. The distal tubule cells (macula densa) sense the Na in the filtrate, and the arterial cells (juxtaglomerular cells) sense the blood pressure. When the blood pressure drops, the amount of filtered Na also drops. The juxtaglomerular cells sense the drop in blood pressure and the decrease in Na is relayed to them by the macula densa cells. The juxtaglomerular cells then release an enzyme called renin. Renin converts angiotensinogen (a peptide, or amino acid derivative) into angiotensin I. Angiotensin I is then converted to angiotensin II by an angiotensin-converting enzyme (ACE), which is found mainly in the lungs. Angiotensin II causes blood vessels to contract -- the increased blood vessel constrictions elevate the blood pressure.
Now let's take a look at how the kidney increases the circulating blood volume. Angiotensin II also stimulates the adrenal gland to secrete a hormone called aldosterone. Aldosterone stimulates more Na reabsorption in the distal tubule, and water gets reabsorbed along with the Na. The increased Na and water reabsorption from the distal tubule reduces urine output and increases the circulating blood volume. The increased blood volume helps stretch the heart muscle and causes it to generate more pressure with each beat, thereby increasing the blood pressure.
The actions taken by the kidney to regulate blood pressure are especially important during traumatic injury, when they are necessary to maintain blood pressure and conserve the loss of fluids.
Your body stores calcium in the bones, but also maintains a constant level of calcium in the blood. If the blood calcium level falls, then the parathyroid glands in your neck release a hormone called parathyroid hormone. Parathyroid hormone increases calcium reabsorption from the distal tubule of the nephron to restore the blood calcium level. Parathyroid hormone also stimulates calcium release from bone and calcium absorption from the intestine.
In addition to parathyroid hormone, your body also requires vitamin D to stimulate calcium absorption from the kidney and intestine. Vitamin D is found in milk products. A precursor to vitamin D (cholecalciferol) is made in the skin and processed in the liver. However, the final step that converts an inactive form of cholecalciferol into active vitamin D occurs in the proximal tubule of the nephron. Once activated, vitamin D stimulates calcium absorption from the proximal tubule and from the intestine, thereby increasing blood calcium levels.
Kidney stones are often caused by problems in the kidney's ability to handle calcium. In addition, the kidney's role in maintaining blood calcium is important in the bone disease osteoporosis that afflicts many elderly people, especially women.
As you can see, the kidneys perform many functions that are important to your body:
- Controlling the composition of your blood and eliminate wastes -- filtration/reabsorption/secretion method
- Influencing blood pressure -- renin secretion
- Helping to regulate your body's calcium -- vitamin D activation
If the kidneys fail to function, then renal dialysis methods (artificial filtration methods) can be used to help you survive by cleansing the blood. This is especially necessary when both kidneys fail. Although you have two kidneys, it is possible to live with only one. One healthy kidney can be donated and transplanted into a compatible person with total kidney failure. Kidney transplants are a common way to help those people survive and live a normal life.
For more information on the kidney, its functions and its diseases, check out the following page.