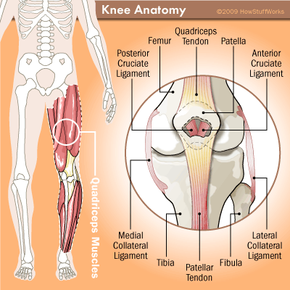
It's the biggest joint in the body, it's more complex than it first appears, and it's fun to bounce soccer balls off of -- it's the knee. Your knee allows your lower leg to be extended outward or pulled back toward your body. It's a crucial part of our ability to move around (lock your legs in a straight position for an hour if you have any doubts). All good things must come to an end, though, and so it is with this meeting of the femur (your thighbone), the tibia (your shin) and the patella (the kneecap).
Most of the time, arthritis (an inflammation of a joint) is the reason why a knee joint must be replaced. However, sports injuries, excessive wear-and-tear and genetics also lead to badly damaged knees. A condition caused by lack of blood flow to the knee, avascular necrosis, also kills bone tissue. Fortunately, advancements in science and medicine enable us to replace this important joint, extending and increasing not only mobility but also the quality of life for people with damaged knees.
Advertisement
Early implant devices were little more than simple hinges, but modern artificial knees come much closer to replicating the knee's unique gliding and rolling motions while providing strength and stability. Hundreds of thousands of people undergo total knee replacement surgery, also known as total knee arthroplasty, all over the world each year -- there are more than 400,000 knee replacements each year in the United States alone [source: Sharpe]. With the population growing and techniques improving, that number will only increase.
Generally, people over 65 make up the largest candidate pool for total knee replacements [source: Arthritis Research Campaign]. The procedure can also performed on younger patients suffering from pain and loss of mobility, though it's best to put off this surgery as long as possible. The life span of an artificial knee is around 10 years. Middle-aged recipients will likely need a second replacement down the road, and the second procedure is often not as successful as the first (we'll talk about why a little later).
In this article we'll discuss why knees need to be replaced, how total knee replacements are performed and what to expect from your new knee.
Advertisement