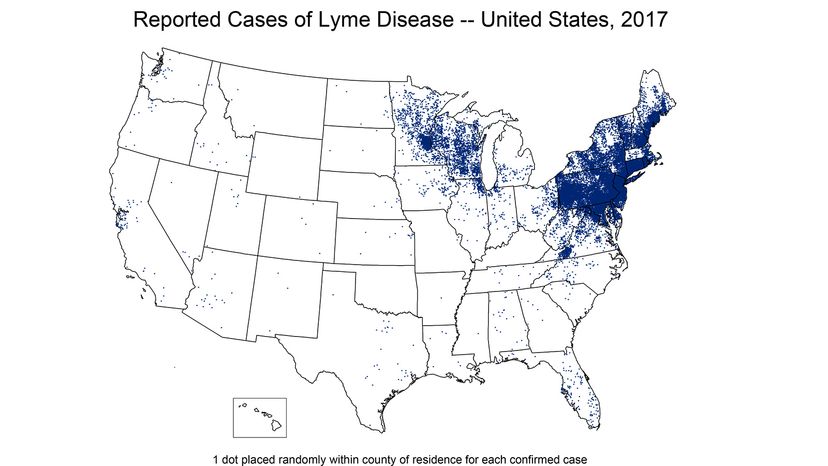
July marks the high season for Lyme disease. If you're in an area of the United States where Lyme is inclined to fester — the mid-Atlantic and northeastern regions of the country mainly, but it's in the north central part of the country, too, and spreading — this time of year might make you a little nervous about being around all those nasty, bitey little ticks that carry the disease.
And news coming from the Centers for Disease Control sounds awful grim. The number of confirmed cases of Lyme disease in the U.S. has more than doubled since 1997, (the most recent year for final figures is 2017) and cases increased 17 percent between 2016 and 2017 alone. While cases used to be mostly isolated to the Northeast, now the CDC considers half of the counties in the United States high-risk for Lyme disease. Did we say the news sounded grim?
Advertisement
The thing is ... take a breath. Calm down. Lyme disease, first identified in the U.S. in the 1970s, is not particularly mysterious or anywhere close to untreatable, despite the horror stories that you may have heard or those message boards — gasp! — that you've read on the internet.
"The problem is that there are a lot of people that think they have Lyme disease that actually haven't," Phillip Baker, the executive director of the American Lyme Disease Foundation, says. "That's a problem."
Lyme disease should not be taken lightly. If you think you may have it,you need to see a doctor. The sooner, as with any sickness, the better. By some estimates, somewhere around 300,000 possible cases of it are diagnosed every year.
But the vast majority of those cases — this is important to remember for the nervous among us — are handled with a simple round of oral antibiotics. If caught early, especially, people recover quickly and completely.
"I don't want to minimize it. Lyme disease is a serious disease. It's important that people that have it get diagnosed properly and treated," Baker says. "But it's not something that's impossible to handle. It's very manageable. It's not an infection that's difficult to treat. In fact, nine times out of 10, if it's diagnosed correctly and treated correctly, people don't have any problems."
Advertisement