It's a scary movie cliché – the good guy does everything he can to kill the bad guy, and no matter what he tries, the bad guy just keeps getting back up, bloody and mangled, but still alive somehow. Eventually, the hero deals one final blow, and the evildoer dies.
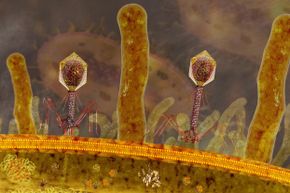
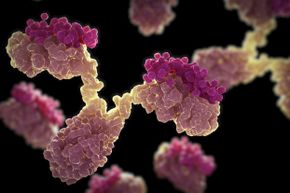
Health care is a lot like these scary movies. Doctors fight the villains – let's say bacteria – with all the tools they have – in our case, a slew of antibiotics. The bacteria fight to live, but eventually the antibiotics prove too powerful. The bacteria and the resulting infection die, and we live. Yay for modern medicine!
Advertisement
But you know how where there's a bad guy, there's always a sequel in the making where he's not really dead? In the health care world, we're moving rapidly toward that same scenario. The bugs that are infecting us are transforming into superbugs, impervious to all known antibiotics. Health care leaders across the globe are warning that many of the bacteria that harm us are growing resistant to the drugs we've been using to combat them, pushing us toward a post-antibiotic world where the bacteria just might win.
What might this world look like?