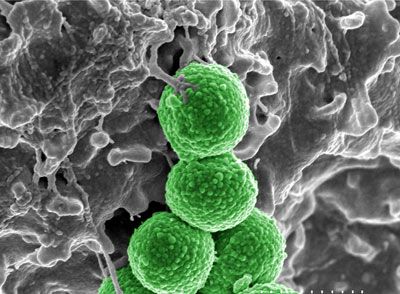
You know when your doctor prescribed a course of antibiotics and told you to take the entire prescription? You really should've listened. Thanks to millions of misused antibiotic prescriptions worldwide (how many half-empty bottles are in your medicine cabinet right now?), the bacteria you intend to kill are getting stronger. In fact, some bacteria -- like the MRSA superbug -- are immune to select antibiotics.
This happens through the process of natural selection. People take antibiotics to wipe out the bad bacteria causing an infection. But some bacteria are stronger than others, and if you don't finish the entire regimen of antibiotics, some bacteria will survive and pass on their resistance to antibiotics.
Advertisement
The evolution of drug-resistant bacteria is not just the result of prescription neglect. Antibacterial and antimicrobial soap, and other cleaning products you have in your bathroom and kitchen, are also responsible. Just as antibiotic prescriptions can be misused, so, too, can antibacterial products. When was the last time you washed your hands for the full 20 seconds that the national Centers for Disease Control suggests? Twenty seconds may not sound like much, but that's as long as it takes to belt out a full version of the ABCs.
Antibacterial and antimicrobial agents were created to prevent the spread of infection in hospitals. But companies began marketing these products to everyday consumers, too. As a result, more microbes are exposed to and develop resistances to these agents.
By using more antibacterial products, people may encourage bacteria to evolve and become more virulent than they were before. Overusing antibacterial products is now a major point of study within the field of pharmacoepidemiology -- the study of how people use medicines.
If antibacterial and antimicrobial products may be a threat to public health, why are are they still on store shelves? We'll get to that, but first let's look at how antibacterial products work -- or don't work.
Advertisement