Sixty years ago, scientists were on the cusp of a revolutionary scientific breakthrough. In the preceding decades, researchers had had some success transplanting organs in animals, and there had even been a few failed attempts at human organ transplants. Numerous studies showed that human organ transplantation was feasible, and that it would be enormously beneficial to thousands of patients, but nobody had been able to make it work.
Success finally came in the early 1950s, when several kidney transplants within a few years gave new life to ailing patients. In the following decades, doctors learned how to transplant other organs successfully, and they dramatically improved recovery rates. Today, most organ transplants are relatively safe, routine procedures, and transplantation is considered to be the best treatment option for thousands of patients every year.
Advertisement
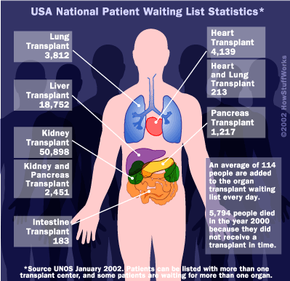
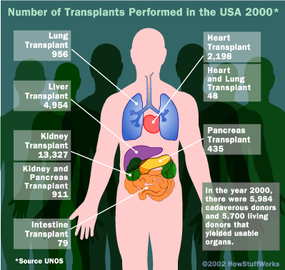
Unfortunately, doctors and patients now face a new obstacle: The demand for transplants has far surpassed the supply of donated organs. Simply put, there aren't enough organ donors, so patients must wait months, even years, for their chance at recovery.
In this article, we'll look the three major processes involved in organ transplantation: the organ distribution system, the surgery itself and the post-surgery recovery. We'll also explore how scientists and politicians are working to remedy the organ-shortage problem.
The Screen, the List and the Match
Organ transplants are one option when a particular organ is failing. Kidney failure, heart disease, lung disease and cirrhosis of the liver are all conditions that might be effectively treated by a transplant. For problems with the heart, the lungs and other highly sensitive organs, a transplant is typically the course of last resort. But if all other avenues have been explored and the patient is willing and able, transplantation is a good, viable option.
Kidneys and livers may be transplanted from a living donor, since people are born with an extra kidney and the liver is regenerative. Even a lung can be transplanted from a living donor, but this is still very rare. For these procedures, a patient will generally find a willing donor in a friend or family member. If the donor is a match, they can proceed directly to the surgery stage. A smaller number of living transplants come from charitable people donating for the general good.
If a patient needs a heart transplant, a double lung transplant, a pancreas transplant or a cornea transplant, they will need to get it from a cadaverous (deceased) donor. Generally, acceptable donors are people who are brain dead but on artificial life support. Even though they are technically dead, their body is still functioning, which means the organs remain healthy. Organs will deteriorate very quickly after the body itself expires, making them unusable for transplant.
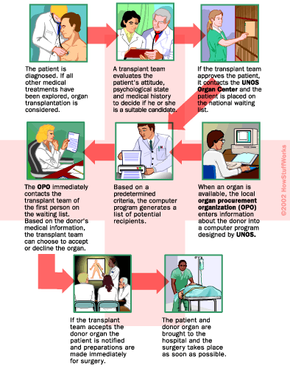
In the United States, a patient who wants an organ transplant from a cadaverous donor must become part of an elaborate nationwide organ distribution system. This system, known collectively as the Organ Procurement and Transplantation Network (OPTN), is operated by the United Network for Organ Sharing (UNOS), an independent nonprofit organization working under contract with the U.S. Department of Health and Human Services.
UNOS maintains a database of eligible transplant patients awaiting organs as well as detailed information on all the organ transplant centers around the country. Additionally, the UNOS board of directors, primarily made up of transplant doctors, transplant patients and organ donors, establishes the policies that decide who will get which organs.
Advertisement