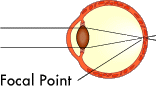
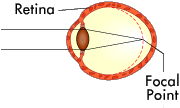
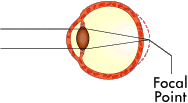
The basis for all laser eye surgery is to reshape the cornea so that it changes the focal point of the eye. Ideally, the focal point is changed so that it focuses perfectly on the retina, just like a normal eye.
As stated in the previous section, myopia (nearsightedness) usually results from the eye being too long. The cornea has a more pronounced curve than a normal eye. Laser eye surgery is great for myopia because it is relatively easy to remove a little of the cornea to flatten out the curve.
Hyperopia (farsightedness) normally means the eye is too short, which means that the cornea needs to curve more to properly focus the light on the retina. Although more intensive than correcting myopia, laser eye surgery can treat hyperopia by reshaping the cornea to make it rounder.
Laser eye surgery works by pulsing a tightly-focused beam of light (laser) onto the surface of the eye. Upon contact with the surface of the cornea, the laser vaporizes a microscopic portion of the cornea (more on this later). By controlling the size, position and number of laser pulses, the surgeon can precisely control how much of the cornea is removed.
LASIK combines the best features of ALK and PRK (see above). Like ALK, LASIK uses a microkeratome to create a "flap" of the outer corneal tissue that can be folded out of the way and then replaced. Once the flap is folded out of the way, LASIK uses the same Excimer laser used in PRK to reshape the underlying corneal tissue. Then the flap is replaced over the reshaped area and conforms to the new shape.
The great thing about the cornea is how quickly it heals. As soon as that flap is replaced, it begins to naturally seal itself to the rest of the cornea. This approach greatly speeds the overall healing process when compared to PRK, which leaves the reshaped area open.
Of course, there are potential problems with LASIK. The three most common problems are:
- Undercorrection - Not enough tissue is removed during the procedure.
- Overcorrection - Too much tissue is removed during the procedure.
- Wrinkling - The corneal flap has a small fold or wrinkle in it when it is replaced, causing a small blurry area in your vision.
Under most circumstances, each of these problems is easily corrected with a second surgical procedure. If the undercorrection or overcorrection is very slight, the surgeon will most likely advise the patient not to attempt to refine his or her vision any further. In fact, many recipients of laser eye surgery never achieve normal vision but are able to reduce their corrective-lens prescription significantly.
In addition to the more common problems listed above, there is a potential for other side effects such as blurred vision, halos around lights, increased light sensitivity and even double vision. There is also the chance that damage or scarring can happen to the cornea, resulting in a partial or complete loss of vision.
These other problems occur only rarely when you're dealing with reputable ophthalmologists operating on patients who meet the parameters of an ideal candidate. We'll talk more about what makes an ideal candidate later.
For now, let's take a closer look at the laser used in eye surgery.