You might not think about your bones very often unless you break one. When you break a bone, the bone heals itself and begins to regrow. But, what if your muscles, tendons and ligaments turned to bone? What if you formed a second skeleton on top of the one you already have? That's what happens with Fibrodysplasia Ossificans Progressiva, or FOP.
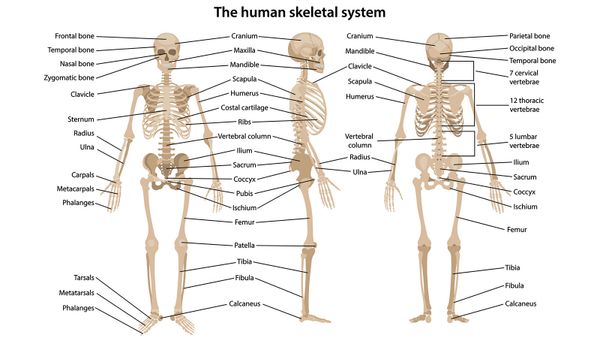
An FOP skeleton doesn't look like the ones you see at Halloween or the kind that hangs in an anatomy classroom. Instead of having lots of bones linked to one another with functioning joints, an FOP skeleton's bones fuse together, essentially forming a second skeleton out of the tendons, ligaments and muscles -- a true metamorphosis. The skeleton is almost one solid piece, and sheets of bone exist where they should not.
Advertisement
The most common sign of FOP can be seen at birth: malformed big toes. Doctors aren't sure why this happens -- it just appears as an early indicator of FOP. Aside from the malformed big toes, other initial signs of FOP usually show up in the first two decades of life. One day, a large lump suddenly begins to form on a child's body, usually in the neck or back area. It can appear rapidly, often overnight, and grows much faster than most tumors. It's warm to the touch, red and painful. A person's first reaction is often to assume it must be some sort of tumor -- what if it's cancer? But then the lump stops being painful, eventually gets smaller, and turns to bone -- normal bone, but in the wrong place -- where the body neither needs it nor wants it.
These lumps are called flare-ups, and they appear all through the life of a person with FOP. Doctors aren't always sure what triggers them, but they do know that any kind of injury, even a small one, can cause a flare-up. For someone with FOP, a fall is not just a fall, and the typical bumps and bruises of daily life are a major threat to the mobility and independence. If a person with FOP bumps his elbow or knee, bone could begin to grow there and lock the arm or leg.
In FOP patients, extra bone formation almost always starts at the neck, spine and shoulders. Only then does it move to the other joints. Eventually, people with FOP will probably lose most of their mobility. Joints lock, and bones can twist into odd positions. Some people with FOP develop scoliosis, and their spine twists. Often, the jaw fuses together either spontaneously or as a result of an injection for dental work, which makes eating and brushing teeth extremely difficult. The skeleton will fuse into one position, and that is the position a person with FOP will stay in for the rest of his or her life. Any attempt to remove the extra (or heterotopic) bone only leads to extra bone formation. Only 700 people worldwide are known to have FOP, which makes this disorder extremely rare [source: IFOPA].
In this article, we'll learn how FOP bone compares to normal bone, how doctors treat FOP and what other kinds of rare bone disorders exist.
Advertisement