In 2014, Brittany Maynard was a vibrant 29-year-old trying to start a family with her new husband when debilitating pain began gripping her head like a vise. The diagnosis: brain cancer. Despite two surgeries to stop the tumor's growth, it roared back more aggressively than ever, and she was soon given a mere six months to live. Faced with a treatment plan of full-brain radiation, which wouldn't cure her yet would burn her scalp, and possibly developing morphine-resistant pain, personality changes and cognitive losses, she opted for medically assisted suicide.
To achieve the death she wanted, Maynard had to relocate from California to Oregon, one of the few states that allows medically assisted suicide. During her final weeks of life, Maynard created a six-minute video about dying with dignity that ignited passions in the U.S. She died as she wished, after taking a lethal dose of sedatives and respiratory system depressants provided by her physician, on Nov. 1, 2014. Less than a year later, thanks to her video and activism, her home state of California passed aid-in-dying legislation. In addition, death-with-dignity legislation was rapidly introduced in half of the states [source: The Brittany Maynard Fund].
Advertisement
Medically assisted suicide generally means a physician prescribes lethal medication to a patient, who ingests the medicine herself. Euthanasia, in contrast, typically refers to a physician administering the lethal medication to the patient.
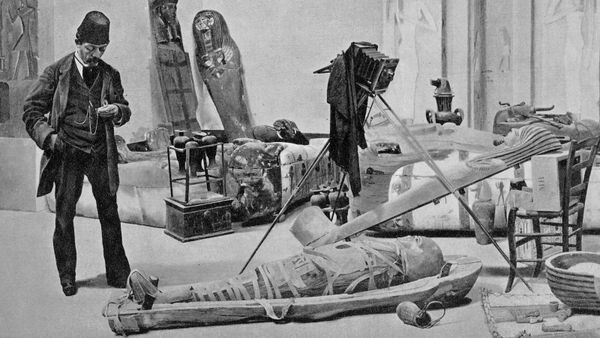
The notion of medically assisted death is hardly a new one. It's been around since ancient times, and goes by various names — medically assisted suicide, physician-assisted dying and euthanasia, although as just noted, the latter is not an accurate term.
Yet despite its longevity, it's been largely spurned around the globe in the modern era. It wasn't until 1940 that Switzerland approved the practice, and nothing much happened after that for decades. More recently, the practice got some traction when Colombia approved physician-assisted death in 1997, followed by the Netherlands and Belgium in 2002, Luxembourg in 2009, England and Wales in 2010 (via a prosecution policy statement) and Canada in 2016 [sources: Assisted Suicide, BBC].
Thanks partly to Maynard, a 2015 Gallup poll showed 68 percent of Americans support the practice, a 10 percent increase from the prior year [source: Dugan]. Yet there's always a bit of unease around legalization — the percentage of Americans who support actual legalization dips to about 50 — as some fear the practice could be abused [source: Quill and Greenlaw].
Let's look at what, exactly, is involved in physician-assisted death.
Advertisement