People with hyperhidrosis can experiment with a variety of treatment methods until they find one that works well for their particular situation and lifestyle. Doctors typically advise patients to start with the simplest, least invasive options available and work their way up as needed.
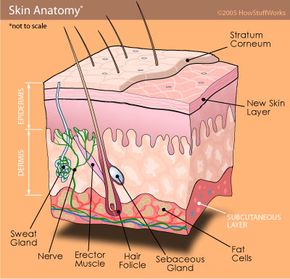
Using antiperspirants is the easiest way to treat sweating. Antiperspirants come in a range of strengths, both over-the-counter and prescription. They work by blocking the duct openings that lead to the sweat glands, preventing sweat from reaching the surface. Their active ingredients are metallic salts, most commonly aluminum compounds such as aluminum chloride hexahydrate, which is popular in prescription antiperspirants. Many people with hyperhidrosis can also use antiperspirants on other parts of their bodies besides their armpits, such as their feet, to lessen sweat production (although this can irritate the skin). To learn more about how this process works, read What is in an antiperspirant that stops sweat?
If antiperspirants don't do the trick, a treatment called iontophoresis is typically the next step. Iontophoresis can be used for palmar, plantar and axillary hyperhidrosis, though no one is really sure exactly how or why the process works. For some people -- possibly as much as 80 percent of those who try it -- iontophoresis provides good results. In many cases, the treatment drastically reduces sweat levels or temporarily stops sweating [Source: International Hyperhidrosis Society].
Reported to have been used as early as 1740 in order to treat arthritis, iontophoresis is a simple process [Source: International Hyperhidrosis Society]. Hands and feet are placed in shallow, water-filled trays, and an electrical current charges the water at a level comfortable for the user. The process sends a light electrical current through the tray contents to ionize the particles in the water, which then pass into the skin. Treatments can be performed by a dermatologist, or people can purchase iontophoresis machines and self-administer treatments at home.
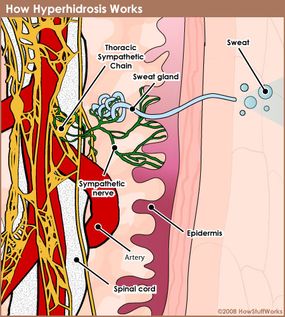
Theories abound as to how the ionized particles interfere with the sweating process. Some ideas are that the ionized particles may plug the sweat gland or interrupt the nerve signal, but as for a definite conclusion, the jury is still out.
Iontophoresis treatments take between 20 and 40 minutes and need to be repeated frequently at first. Over time, follow-up treatments may be needed only every week or every month, depending on the person. Padded electrodes can be used to treat armpit sweating, too.
People with hyperhidrosis who may want a more low-maintenance treatment --albeit one that's more expensive -- can get Botox injections to stop sweat production in their armpits. In both the U.S. and the U.K., Botox has been federally approved for the treatment of axillary hyperhidrosis, although it can also be used on the feet, hands and face. Botox, a purified botulinum toxin protein, blocks the nerve endings that would signal the sweat glands into overdrive. The length of time Botox injections can stay effective ranges from three to 16 months. Follow-up injections may be needed soon after the primary one, if some spots were missed.
Other lines of attack include astringents and topical or oral medications.
More invasive treatment options exist for those who have severe hyperhidrosis and seek more permanent relief. We'll examine those next.