Archeological findings reveal that amputation procedures have been performed since ancient times. The earliest amputations, though, were performed mainly to remove tissue that was already dead. The reason for this limitation is that early surgical techniques could not control the blood loss, called hemorrhaging, that results from cutting healthy arteries.
Surgeons in ancient Greece and Rome dealt with the problem of hemorrhaging by introducing the technique of tying off, or ligating, blood vessels during surgery. Surprisingly, their techniques appear to have been forgotten for many centuries. It was during these times that blood vessels were instead cauterized using hot irons or boiling oil.
Advancements in amputation surgeries have tended to follow major wars. The techniques introduced by French military surgeon Ambroise Paré are a good example of this. Due to the rise of gunpowder and the weapons of war associated with it, Paré needed more effective methods of treating soldiers with devastating battlefield injuries. Among his several important contributions, Paré reintroduced the technique of ligating blood vessels
in 1529.
Other notable advancements throughout history include the introduction of the tourniquet in 1674, which enabled further control of blood flow during the amputation procedure, and one more innovation that patients undoubtedly appreciated -- anesthesia. It's hard to imagine, but anesthetic gases weren't developed until the 1840s.
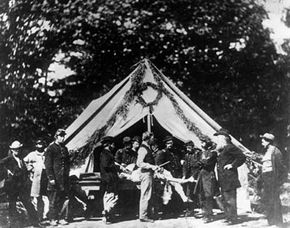
These developments were all put to extensive use during the American Civil War, in which more than 50,000 amputations were performed. The lead Minie ball bullets of this era pulverized tissue like no weapon before, explaining why 75 percent of all battlefield surgeries were amputations.
By today's standards, battlefield amputations of the American Civil War were primitive. For one thing, the concept of maintaining a sterile environment, free from germs, had not been developed. Blood-spattered surgeons often operated without so much as washing their hands, barely taking the time to rinse off their tools between surgeries. The focus was instead on speed. To cycle through as many patients as possible, the surgeries were performed quickly -- usually in about 10 to 15 minutes.
The surgeon would knock out the patient with a chloroform-soaked rag, and then quickly apply a tourniquet above the injury site before using a sharp knife to slice through the skin and muscle. The bones were next sawed through -- earning Civil War surgeons the nickname "Sawbones" -- and the blood vessels were tied off with sutures. Finally the skin was closed around the amputation site, leaving a hole from which fluid could drain. Infamously, the amputated limbs were thrown out, building up in great piles.
Death rates after the surgeries were dismal by today's standards. In fact, one out of four patients died after a typical amputation, but the mortality rate doubled if the surgery wasn't performed in the first 24 hours. The deaths were caused in part by bacterial infections termed "surgical fevers" resulting from the non-sterile surgeries. It was only just after the Civil War that British surgeon Joseph Lister advanced the concept of sterile surgery. Nevertheless, thousands of lives were saved by the round-the-clock efforts of the American Civil War surgeons.
Since historical times, great advancements in amputation techniques have been made. On the next page, find out how surgeons and patients prepare for modern day amputation surgery.