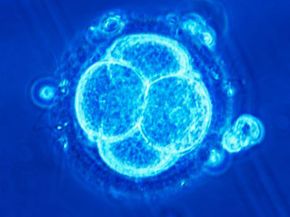
Infertility, defined as the inability to become pregnant after one year of unprotected sex, is a problem faced by nearly 6.1 million Americans -- that's nearly 10 percent of men and women of reproductive age [source: eMedicineHealth]. Because this problem is so prevalent, fertility treatments abound. Assisted reproductive technology (ART) is a group of fertility treatments that involve both the sperm and the egg. In vitro fertilization (IVF) is the most common type of ART. In IVF, the sperm fertilizes the egg outside the body, and doctors implant it into the woman's uterus in hopes of a successful pregnancy. Other forms of ART include intracytoplasmic sperm injection (ICSI), gamete intrafallopian transfer (GIFT) and zygote intrafallopian transfer (ZIFT).
The history of IVF is relatively short. Louise Brown of England was the first baby born via IVF, in 1978. The next IVF baby was born later that same year in India. Soon, people started calling these infants "test-tube babies." In 1981, the first American test-tube baby was born, and the number has continued to increase each year. According to the Centers for Disease Control, more than 48,000 babies were born in 2003 through ART -- 99 percent of these with IVF [source: CDC].
Advertisement
People just starting the fertility process -- if the woman doesn't have severely damaged fallopian tubes -- usually attempt other treatments before IVF. Depending on the source of the problem, women can take antibiotics, fertility drugs or prescription hormones to increase the chances of pregnancy. Surgery could be the answer for women who suffer from structural problems in the fallopian tubes or uterus. On the male side of the equation, one option is medication that increases sperm production. Men can also take antibiotics and prescription hormones or try a few lifestyle changes, like wearing looser underwear and avoiding hot showers and saunas.
If these treatments don't work, artificial insemination may be the next step. In this procedure, the sperm (from the male half of the couple or a sperm bank) is collected and manually placed in the woman's uterus or fallopian tubes. Another pre-ART option is intrauterine insemination, or IUI, where the sperm is placed directly into the woman's uterus using a catheter, which gives the sperm a head start in the race to the egg.
It's usually when all else fails that people turn to ART treatments, and most use IVF. People are most likely to use IVF when low sperm count or blocked or damaged fallopian tubes are the culprit. Women who suffer from endometriosis may also benefit from IVF treatment.
Now that you have a general idea of IVF, let's get into the specifics. In the next section, we'll explain the fertilization process.
Advertisement