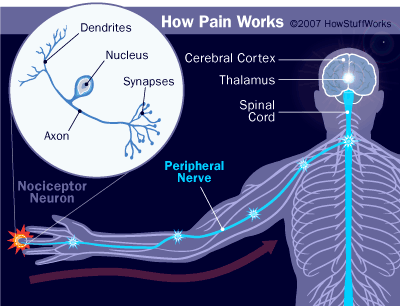
It often begins so innocently -- just a vague sensation of slight pressure around your temples. But soon it intensifies. Before long, it feels as if your head is being squeezed like a stress ball. The pain makes it difficult to focus and starts to affect your mood as well. Only after several hours (and a few pills) does the headache finally subside.
The scenario just described is all too common for the many people who deal with tension headaches. And those who only get this type of headache are the lucky ones. Imagine, for example, the experience of a migraine headache. Strange distortions to your vision might come first as a warning sign, and then the full attack commences. Once the throbbing head pain and nausea are in full swing, resting in a dark room is all you'll feel like doing.
Advertisement
The pain of cluster headaches is even more intense, commonly described as the feeling of a hot poker being stuck into the brain through one's eye socket. Cluster headaches get their name because they come in repeated bursts, with each burst being so excruciating that unlucky victims can often do nothing but pace around in agony.
As opposed to primary headaches, such as the types of headache described above, secondary headaches arise from an underlying injury or illness. For example, a blow to the head can cause internal bleeding that increases pressure within the brain, creating an intense headache. Because secondary headaches can indicate a serious underlying problem, they should never be ignored
So how do you know when it's time to see the doctor about a headache, and what are the different types of headaches it might be? Also, why do headaches hurt in the first place, and how can they be treated?
Let's start on the next page by taking a closer look some of the major headache types.
Advertisement