All it takes is just one drop of Salmonella-contaminated liquid from improperly handled or stored raw chicken to contaminate another food or liquid. That contamination can happen either through direct contact, or indirectly through contaminated kitchen utensils or cutting boards. About 48 million people — that's about one in six, and most under the age of 5 or over 65 — get sick with a foodborne illness every year in the U.S. Of those, 128,000 are hospitalized, and 3,000 die [source: NIAID].
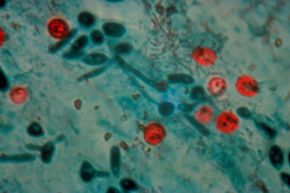
Foodborne illnesses are caused by different types of pathogens, including commonly thought-of sources such as bacteria, viruses and parasites, in addition to the ones that don't come to mind as often, such as pollutants and toxins. The most common foodborne pathogens are Salmonella, responsible for 38 percent of reported foodborne infections, followed by Campylobacter, responsible for 35 percent of reported infections. Both of those cause gastrointestinal problems and fever, and both are usually self-limiting, lasting about 10 days or less.
Advertisement
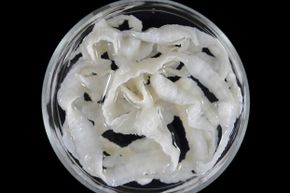
While none of that sounds like a good time, here we have 10 foodborne illnesses that do more than keep you on the bathroom floor for a night or two. These pathogens paralyze your muscles, cause explosive and watery diarrhea, and may even make you think hot feels cold and cold feels hot.