Once a donor and recipient have been matched and the associated legal and preliminary medical criteria are complete, the women begin a multi-step medical process before egg harvesting.
The donor and recipient's menstrual cycles must first be synchronized. Synchronization involves many steps, and donors are taught to administer their own medications -- both through injections and pills. On the first day of menses, a physician assesses the donor's ovarian function through blood tests and a vaginal ultrasound, and the donor begins taking birth control pills.
The next step is to suppress the donor's natural ovulation. This is managed through daily injections of gonadotropin (GnRH) agonists that shut down hormones secreted naturally by the pituitary gland. A cycle takes about four weeks, and in addition to birth control pills and GnRH agonist injections, a donor undergoes routine blood tests and vaginal ultrasound examinations to monitor progress. To bring this cycle to an end, the donor stops taking birth control pills and has a menstrual period that is synched with the recipient's cycle.
During the process's next stage, the ovarian stimulation process, the donor injects herself with hormones to help stimulate the release of multiple mature eggs. Normally, women release only one egg each month. The recipient also uses medication to suppress her own ovulation and to thicken the lining of her uterus for upcoming embryo implantation.
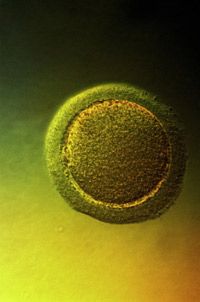
During the ovarian stimulation phase, the donor undergoes frequent blood tests and ultrasounds to monitor egg follicle development. When the follicles are fully developed, the donor injects herself with human Chorionic Gonadotropin (hCG), helping her eggs separate from the follicle walls for retrieval. At this time, the recipient adds progesterone injections to her list of medications that prepare her body for the embryo transfer.
The timing of the hCG injection is crucial to successful egg retrieval, and eggs are collected about 34 to 36 hours after the hCG injection by ultrasound-guided needle while the donor is under anesthesia [source: WebMD].
The harvested eggs are combined with sperm -- either from a sperm donor or from the recipient's husband or partner -- and after a few days of incubation, two to four embryos are placed in the recipient's uterus via a thin tube inserted through her cervix [source: CDC]. This is in vitro fertilization (IVF).
Typically, all the eggs harvested in a cycle are inseminated. If there are any remaining embryos, they legally belong to the recipient and can be saved through cryopreservation for future pregnancy attempts.
Egg donation is not risk-free. Medications used to synchronize menstrual cycles sometimes cause hot flashes, mood swings and breast tenderness. Also, the medications used during the ovarian stimulation process may cause ovarian hyperstimulation syndrome (OHSS), fluid retention and swelling of the ovaries. There are varying degrees of OHSS, from mild abdominal pain to life-threatening blood clots. However, with careful monitoring, a donor has less than a one percent chance of developing severe or life-threatening OHSS [source: WebMD]. Long-term risks of egg donation and ART are unknown but a link between fertility drugs and an increased risk for ovarian cancer is being studied [source: Department of Health, State of New York].
In recent years, regulations and guidelines have gone into effect concerning donor cells and tissues, procedures and compensation. As part of the FDA's "Good Tissue Practices," clinics are required to test donors for infectious diseases and maintain accurate records. Additionally, the American Society for Reproductive Medicine's (ASRM) Ethics Committee reports that compensating donors more than $10,000 is unreasonable and risked coercion. As we've learned, ASRM recommends women be compensated no more than $5,000 [source: ASRM].
For more information about pregnancy, infertility and assisted reproductive technologies, visit our list of links on the following page.