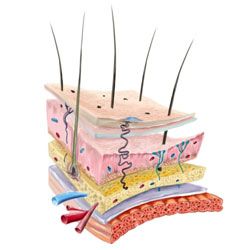
Despite its comparative toughness and impressive size, many problems can plague the skin. Ultraviolet radiation from the sun can damage the DNA in skin cells, leading to sunburn or even cancer. The effects of dry and windy climates can wick moisture from skin, leading to chapped, painful areas. Sebaceous glands can become clogged, which can cause pimples.
There are certainly measures we can take to prevent damage to our skin from environmental exposure. But there are also skin disorders that take place from the inside and are the result of genetic mutations that we can inherit from our parents. These inherited skin problems are collectively referred to as genodermatoses, or genetic dermatological disorders.
Advertisement
The range of genodermatoses is sweeping. Some, like psoriasis, can be relatively mild and treatable with topical remedies. Others, like harlequin-type ichthyosis, can be fatal. What follows are five inherited skin problems that cover a lot of epidermis.