Not everyone suffering from obesity is eligible for weight-loss surgery. While guidelines can vary from surgeon to surgeon, the National Institutes of Health (NIH) has set a few standard criteria for screening patients for surgery. Those patients whose body mass index (BMI) is between 35 and 40 can be considered if they are also suffering from a complication caused by their obesity, such as diabetes. For patients with a BMI of more than 40, no complication is required for approval.
Beyond the BMI qualifications, patients must have been obese for more than three years and have attempted to lose weight through diet, exercise and medications without success. Because weight gain is often a result of psychological factors, patients must have a psychiatrist's clearance before they can have the surgery. Psychological criteria include assessments for any self-destructive behaviors, depression or substance abuse. While strict, these criteria are essential in order to ensure the success of the surgery and, ultimately, the weight loss.
While doctors do not typically perform gastric bypass surgery on adolescents, certain situations may make surgery necessary. Doctors may consider surgery for adolescents who have a BMI of 40 or more, have tried to lose weight for at least six months, have severe complications as a result of their obesity and have reached their adult height. Boys usually reach adult height around the age of 15, girls around age 13.
The Risks
Gastric bypass surgery has some of the same risks as other surgeries, including infection of the incision site, excessive blood loss and blood clots. The procedure also has its own specific risks, including the development of gallstones, stomach leaks, hernias and bowel blockages. In some cases, the newly made connection between the stomach and the intestines can tighten. This narrowing often results in nausea and vomiting directly after a meal.
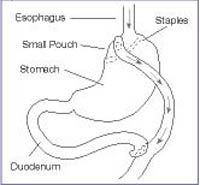
The most common complication is malnutrition. Because food travels directly from the stomach pouch to the middle of the small intestine, the patient absorbs fewer calories and fewer nutrients from food. This can often result in a lack of iron, calcium or vitamin B12 in the body, leading to anemia and osteoporosis. Because this risk is dangerous, doctors require most patients to keep a journal of what and how much they eat each day. This food journal allows doctors and nutritionists to make sure the body is absorbing enough of the right nutrients.
Some patients can also suffer from what is known as dumping syndrome. This complication is a result of food moving too quickly through the body. It can cause the patient to feel nauseated, sweaty and faint. Eating sweets may cause extreme weakness and diarrhea. Sugar tends to be especially irritating due to its high osmolarity. This is a measure of osmotic pressure, which relates to the speed at which fluids travel through a membrane. When these foods arrive in the small intestine, they draw lots of fluid into the intestine along with them. The intestine tries to move them out of the body quickly in an effort to regain balance of intestinal fluids, which is why the cramping and diarrhea can happen. Patients who have undergone gastric bypass surgery should stick to natural sugars like those found in fruits, which do not usually cause dumping syndrome.
Other complications can occur if the patient does not stick to the required diet after the operation. Eating too much food can result in the staples pulling loose and the stomach returning to its original size. Replacing the staples requires an additional surgery.
Finally, there is a risk of death with gastric bypass surgery. The risk varies with the age and overall health of each patient. In general, the likelihood of death ranges from 0.3 percent to 1.0 percent.
Now we'll take a look at what happens before the surgery.